
11 Mar Diet and pregnancy, it’s not about “eating for two”
Pregnancy is one of the most beautiful, exciting and challenging stages in a woman’s life. It’s also one where diet and proper nutrition are vital, not only for the well-being of the mother, but also for the normal growth of the baby.
Fortunately, we have already left behind the concept that a proper nutrition in pregnancy was equal to “eating for two,” where attention was paid to the quantity of food rather than the quality. Likewise, recently it was discovered that certain nutrients have a huge effect and are vital in ensuring the essential functions in the development of the child and in pregnancy outcomes.
Let’s talk about them in a moment, after talking briefly about weight gain.
HOW MUCH WEIGHT SHOULD I GAIN DURING PREGNANCY?
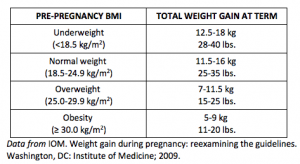
According to the United States IOM (Institute of Medicine), maternal weight gain is linked to the pre-natal nutritional status, or in other words, the Body Mass Index (BMI), before getting pregnant. This means that underweight and normal weight women should have greater weight gains than overweight or obese mothers, just like we can see in the following table:

* Photo credit https://www.healthymummy.com/budget-lunches-under-400-calories/
Remember, it’s vital to maintain a healthy body weight before gestation and appropriate weight gain when you’re already pregnant. If the mother is underweight, overweight or obese, there can be greater health risks to both the mother and the baby.

* Photo credit http://dish.allrecipes.com/main-dish-summer-salads-under-400-calories/
When it comes to eating and extra calories needed for pregnancy, during the first trimester there is minimal need for extra calories. As the second and third trimesters progress, approximately 350-450 extra calories are needed from your pre-pregnancy energy needs. I’ll add some pictures to this blog for you to visually see what that means, but it equates to about an extra snack or light meal in second trimester and an extra 2 snacks or an extra “normal” healthy meal in third trimester.
* Photo credit https://www.lifehacker.com.au/?r=US
EATING RIGHT DURING PREGNANCY
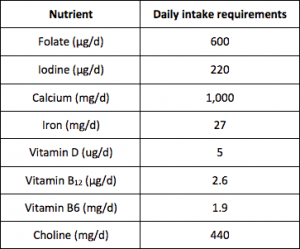
Compared to the need for calories, the importance of vitamins and minerals increases much more. There are key micronutrients (like folate, iodine, calcium, vitamin D and iron) where requirements cannot be met by consuming food alone. You must take supplements plus enhance the quality of your diet as the best choice, rather than increasing portion sizes or the amount of food consumed.
FOLATE
Folic acid or its active form folate (L-methylfolate, also called 5-methyltetrahydrofolate) is considered one of the most important nutrients during pregnancy. It not only supports growth and brain development, but more importantly, prevents neurological defects in the baby. It is universally agreed that every mother should take folate supplements, because the increased needs are very unlikely to be met by diet alone.
Supplementation should begin at least one month before conception and continue through the first trimester of pregnancy. There is still debate and ongoing research on the need for folate in later trimesters, as it was suggested by researchers from the University of Adelaide, that there may be a possible link between taking folic acid supplements beyond the first trimester and the risk of allergies in the child.
Folate supplementation plus a consumption of rich foods like green leafy vegetables, legumes, whole grain products and enriched foods (ie. Wheat flour/breads in Australia have folate added to them), will help you to meet the requirements of this nutrient.
CHOLINE
Along with folate, choline has been found to be an essential nutrient during pregnancy, and later in lactation. Like folate, choline has key roles in fetal development, particularly the development of the central nervous system, the brain and cognition. Of vital importance, is the protective role on neural tube closure. This means that a woman taking a diet high in choline will diminish the neural tube defect risk in her baby. Choline can also permanently change, in a good way, the genetic expression of your growing baby, by affecting lifelong memory enhancement.
Consequently, it’s recommended to increase consumption of choline-rich foods as an excellent strategy to improve the unborn child’s health. Although human requirements for choline are not very clear yet, it has been estimated that a daily intake of 450 mg for pregnant women is needed, which can be difficult to reach with just food alone.
Choline can be found in both animal and plant foods; however, animal sources have significantly more choline; eggs, salmon, and beef steak are the best sources! 2 eggs a day with the yolk will meet about half the daily dietary requirements of choline. But if you prefer plant-based foods you should definitely go for brussels sprouts, broccoli and kidney beans. The most bioactive supplement should contain choline bitartrate or sunflower lecithin.
IODINE
You should also take an iodine supplement, even if you use iodized salt for cooking, because just a mild deficiency can cause negative effects in the baby, like impaired brain and cognitive development. This mineral is also necessary for the development of organs and tissues, and to produce fetal thyroid hormones. Besides from iodized salt, this nutrient can be found in commercially fortified products, and seafood which are naturally rich in iodine and should be eaten twice weekly. Other fruits and vegetables, milk, eggs and then meat can have iodine in variable amounts.
IRON
Iron is the mineral that helps to support fetal and placental growth. During pregnancy, iron requirements progressively increase, being particularly important in the second and last trimester. Inadequate amounts during pregnancy make pregnant mothers at greater risk of anemia, which may affect growth and development of the child and increase the risk of preterm delivery, low birth weight and post-partum hemorrhages.
Food sources of iron are very common and well known: red meat, meat products and fish; but you can also find it in legumes and green leafy vegetables, to enhance the absorption of iron in these foods, you should simultaneously consume vitamin-C rich foods, such as fruit, add tomatoe or lemon juice in the meal (after cooking), or drink orange juice.
CALCIUM
It’s very important to get enough calcium during pregnancy, given that this mineral supports the development and integrity of the bones. Dairy and derivatives are the main sources, but you can also find it in green leafy vegetables, fortified soy products or cereals, almonds, and sardines when they are consumed with bones. If you get enough calcium during pregnancy, you’ll have a reduced risk of preterm delivery, better blood pressure, and may also help with your baby’s birth weight. Most women generally reach their nutrient requirements from food, however, other nutrients that are needed for the absorption of calcium or to aid calcium in building bones, such as Vitamin D, K2 and magnesium are often not consumed in adequate amounts for the pregnant woman’s needs.
VITAMIN D
The much talked about important vitamin D! Vitamin D is obtained from the diet, but is mainly synthesized in the skin during exposure to sunlight (90% of Vitamin D in the body is sourced from the sun). You can find this vitamin in many forms, but the most important of them is vitamin D3 or cholecalciferol. This vitamin will help calcium to exert its function and improves its absorption. Pregnant mothers who rarely spend time in the sunlight, cover their skin or use sunscreen creams, as well as women with darker skin should supplement their diet with vitamin D. You can obtain it in little amounts through foods like egg yolk, oily fish and liver, however, it is unlikely to meet the requirements needed during pregnancy. Vitamin D deficiency during pregnancy puts you at higher risk for preeclampsia, having a low birth weight infant, and gestational diabetes.
WHICH OTHER NUTRIENTS SHOULD I BE PAYING ATTENTION TO?
DHA (docosahexaenoic acid) and Vitamin B12 are other nutrients that have been found to play important roles in maternal nutrition. The first one, DHA, is an essential omega-3 fatty acid, critical for brain and retinal development of the baby right up until they are 2 years of age, that is why it is advised to consume 2–3 servings of fish per week, preferably oily fish like mackerel, herring, sardines or salmon; eating fish twice per week is generally safe and are not associated with risks of toxicity by methyl-mercury. Of note, flaxseed is NOT a source of DHA and the only plant based source of DHA is algae, however, the levels of DHA will be dependent on the species, so it is best to use an algae-based DHA supplement if you dislike seafood.
And lastly, we have Vitamin B12 or cyanocobalamin, which is essential for the formation of red blood cells, and for normal neurological function and the development of the nervous system of the baby. Animal products are the main source of this vitamin and this is why mothers who stick to a vegan and even vegetarian (lacto-ovo) diet, will need to supplement with B12 right through pregnancy and breastfeeding.
And just before ending, I want to illustrate in the next table, what are the recommended Australian intakes of these nutrients for adult pregnant women:
REFERENCES:
1. Committee to Reexamine IOM Pregnancy Weight Guidelines: Weight Gain during Pregnancy: Reexamining the Guidelines. Washington, Institute of Medicine & National Research Council, 2009.
2. Koletzko, B., Bauer, C., Bung, P., Cremer, M., Flothkötter, M., & Hellmers, C. et al. (2013). German National Consensus Recommendations on Nutrition and Lifestyle in Pregnancy by the ‘Healthy Start – Young Family Network’. Annals Of Nutrition And Metabolism, 63(4), 311-322. http://dx.doi.org/10.1159/000358398
3. Marangoni, F., Cetin, I., Verduci, E., Canzone, G., Giovannini, M., & Scollo, P. et al. (2016). Maternal Diet and Nutrient Requirements in Pregnancy and Breastfeeding. An Italian Consensus Document. Nutrients, 8(12), 629. http://dx.doi.org/10.3390/nu8100629
4. Kominiarek, M., & Rajan, P. (2016). Nutrition Recommendations in Pregnancy and Lactation. Medical Clinics Of North America, 100(6), 1199-1215. http://dx.doi.org/10.1016/j.mcna.2016.06.004
5. Hanson, M. A., Bardsley, A., De-Regil, L. M., Moore, S. E., Oken, E., Poston, L., Ma, R. C., McAuliffe, F. M., Maleta, K., Purandare, C. N., Yajnik, C. S., Rushwan, H. and Morris, J. L. (2015), The International Federation of Gynecology and Obstetrics (FIGO) recommendations on adolescent, preconception, and maternal nutrition: “Think Nutrition First”#. International Journal of Gynecology & Obstetrics, 131: S213–S253. doi:10.1016/S0020-7292(15)30034-5
6. Caudill, M. (2010). Pre- and Postnatal Health: Evidence of Increased Choline Needs. Journal Of The American Dietetic Association, 110(8), 1198-1206. http://dx.doi.org/10.1016/j.jada.2010.05.009
7. Folic acid late in pregnancy may increase childhood allergy risk. (2018). Adelaide.edu.au. Retrieved 5 March 2018, from https://www.adelaide.edu.au/news/news97282.html
8. Nichols, Lily. (2018). Real Food for Pregnancy: The Science and Wisdom of Optimal Prenatal Nutrition.
9. NHMRC. (2018) Ministry of Health, Australian Government. Retrieved 13 March 2018 from https://www.nrv.gov.au/nutrients



Sorry, the comment form is closed at this time.