
11 Feb When you love food, but your body doesn’t!
Have you ever felt an awful abdominal pain after drinking a glass of milk? Are you getting more concerned about that sudden rash on your child’s skin when they eat those yummy peanut butter biscuits? Is your baby doing some weird pooey nappies?
It’s hard to see the difference between all these conditions when their symptoms are so alike! You have even tried to ask Dr. Google about it to see a little light, but that hasn’t been any help either.
Let’s continue reading and try to unravel the confusion.
FIRST THINGS FIRST, WHAT IS AN ADVERSE FOOD REACTION?
The Encyclopedia of Gastroenterology describes it as an undesirable physical response to an ingested food product. That means there is a cause-effect relationship between the ingestion, contact, inhalation of a food and an abnormal response in your body. Such responses can affect your gastrointestinal tract, airways, skin, or in the worst cases compromise several organs all at once.
Adverse reactions are more common than you may imagine, however, the severity of the symptoms and clinical manifestations will depend on the type of disorder we’re talking about.
For example, when the adverse reaction happens only to susceptible individuals, we are talking about food intolerances and allergies. In Australia and New Zealand, allergies are common and increasing with 1 in 5 people experiencing allergies in some form (mild to severe) at some point in their life.
FOOD INTOLERANCES AND ALLERGIES ARE OFTEN CONFUSED, SO DON’T THINK YOU’RE THE ONLY ONE!
The main difference you need to know between these two conditions, is that food intolerance usually comes with mostly non-life-threatening digestive issues, does not involve the immune system, nor does it show up on allergy testing. Whereas, food allergy can indeed be life-threatening due to the immune response initiated, if it is not treated promptly.
A classic example of intolerance is the one of lactose. Have you ever asked yourself why some people needs to take lactose-free milk? It’s because their gastrointestinal system does not have an enzyme called lactase, which is a specific enzyme needed for the digestion of the lactose, the type of sugar found naturally in animal milk and other dairy products. Other naturally found sugars such as, fructose, sorbitol, galactose etc, or disorders such as phenylketonuria, and homocystinuria are examples of enzymatic causes of food intolerance, but they are extremely rare and some of them are due to genetic causes.
Food intolerance symptoms often take up to 2 hours to a couple of days to emerge after you eat the food, and possibly include abdominal pain, bloating, flatulence, diarrhoea (ie. mucus, frothy, green or abnormal colour), steatorrhea (oily/fatty stools), with children also exhibiting poor growth or malnutrition.
The treatment for food intolerance is the avoidance of that particular food, although, there are specific treatments for some kinds of food intolerances. Please speak to an Accredited Practicing Dietitian on how to find out what foods you or your child might be intolerant too without eliminating large amounts of food groups or restricting too many foods that may start affecting the growth and nutritional health of you and your child.
And finally, we have allergies, which are an adverse reaction where an immune response is involved. During an allergic food reaction, your body’s immune system confuses specific food components (or in medical terms an allergen) as a threat. In response, it reacts by producing antibodies, which are what fight off the intruder, causing the allergic symptoms.
We have all read stories where something as simple as a person inhaling peanut dust can cause a reaction and make them sick, now you know that it was triggered by the immune system, while defending the body against any possible harm.
ALLERGIES ARE BROKEN DOWN INTO IGE AND NON-IGE MEDIATED ALLERGIES
There are also different types of allergies, according to the EAACI (European Academy of Allergy and Clinical Immunology), allergies can be classified into those that are IgE-mediated, those that are non-IgE mediated and those that are a mix of both. This might seem confusing, but it’s important for you to know what this means, because the severity of the symptoms depends on which one your child has. We’re going to discuss the first type in this first allergy blog series and non-IgE mediated responses in a future blog.
The IgE-mediated food allergies are the ones that may produce immediate symptoms, within minutes to a couple of hours after ingesting the food. These are very dangerous and can potentially lead to anaphylaxis or anaphylactic shock. This is the most serious allergic reaction and it involves multiple organs and systems and can rapidly become life-threatening.
These types of allergies typically appear within the first 2 years of life and most children, by the time school starts will tolerate the foods they are allergic to, including cow’s milk, eggs, wheat and soy; but, peanuts, tree nuts and shellfish are more stubborn, and their tendency for allergic responses usually persist into adulthood – only 10% of children will grow out of tree nut allergies and 20% out of peanut allergies.
Below is a simplified table to help you understand the symptoms between the two:
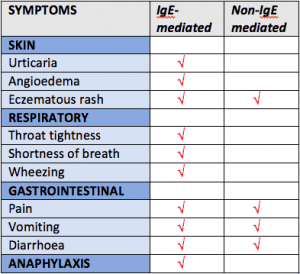
Adapted from DAA and ChildD Paediatric Dietitian training materials 2017
WHAT ARE THE SYMPTOMS OF IGE-MEDIATED ALLERGIES?
Allergies that are IgE mediated can have a wide variety of symptoms. The most common in children are the ones affecting the gastrointestinal tract such as:
- nausea,
- abdominal pain,
- vomiting
- or diarrhoea (mucus, abnormal colours, blood stained, frothy).
The gastric manifestations are usually followed by skin problems like:
- flushing,
- erythema (redness),
- itching,
- urticaria (hives or red itchy rashes),
- eczema
- or angioedema (swelling),
and the airways can be compromised too, with symptoms like:
- oral tingling,
- lip/tongue swelling,
- cough,
- inflammation,
- wheezing,
- and runny nose.
Respiratory disorders are rarely present as the only symptom and usually show up along with gastrointestinal and skin disorders.
In the more severe cases the allergic reaction can lead to anaphylaxis, which usually involves more than one organ and can potentially cause death if it is not treated.
HOW DO YOU TREAT OR MANAGE FOOD ALLERGIES?
The current management of food allergies consists of teaching the patient to completely avoid eating the problem food containing the allergen, as the lowest amount of allergen can trigger all the responses seen above. It’s important as well to involve the family and daycare or school when we’re talking about children and teaching them how to manage in case of an unintended ingestion.
So, if you suspect your child has some sort of allergy, then talk to your doctor immediately to be seen by an Allergist for appropriate specific testing (skin prick test (SPT). They will work closely with you and a Dietitian to start a proper treatment for you or your child. If there is a waiting list to see the Allergist and you are concerned, talk to your GP about having the serum specific IgE blood test (RAST) done. This can test for blanket food group reactions, however a skin prick test will be needed as follow up to find out which specific foods may need to be avoided. If the RAST is negative, there is no IgE-mediated allergy, but there could be non-IgE mediated allergies that need to be further investigated. We will talk more about non-IgE mediated allergies in the coming blogs.
ASCIA can give you more information on the different types of allergy testing available: https://www.allergy.org.au/patients/allergy-testing/allergy-testing , and those that are not appropriate: https://www.allergy.org.au/patients/allergy-testing/unorthodox-testing-and-treatment
References:
* Food Allergy (ILSI Europe Concise Monograph Series). William F. Jackson. Published by International Life Sciences Institute. 2003
* Differentiating food allergies from food intolerances. Guandalini S, Newland C. Curr Gastroenterol Rep. 2011 Oct;13(5):426-34. https://www.ncbi.nlm.nih.gov/pubmed/21792544
* Food allergy. Sampson, Hugh A. Journal of Allergy and Clinical Immunology, Volume 111, Issue 2, S540 – S547 http://www.jacionline.org/article/S0091-6749(02)91253-4/abstract
* IgE-mediated food allergy diagnosis: Current status and new perspectives. Asero R, et al. Mol. Nutr. Food Res. 2007,51, 135 – 147
https://www.ncbi.nlm.nih.gov/pubmed/17195271
* Food Allergies Part 1 lecture notes. National Paediatric Dietetic Training. Dietitians Association of Australia (DAA) & Child Health in Life and Disease Dietetics (ChildD). March, 2017.
* Australian Society of Clinical Immunology and Allergy (ASCIA). February, 2017. https://www.allergy.org.au/patients/about-allergy/what-is-allergy https://www.allergy.org.au/patients/food-other-adverse-reactions/food-intolerance
* Photo credit from http://thegoodshiplollipop.blogspot.com.au/2010/07/allergy-testing.html



Sorry, the comment form is closed at this time.